Oscillate, Expectorate, Ventilate – Repeat
Our cardiopulmonary system has a built-in mechanism that upon sensing mucus production in the lungs, reflexively removes them. That built-in mechanism is often sufficient for individuals with normal lungs that may be infected with an acute infection, however, for those with compromised lungs due to chronic illness, it becomes a much greater endeavor to clear secretions. What can help? Innovative thinkers over time have designed mechanical devices to mimic the natural built-in mechanism of secretion removal.
For compromised lungs that are symptomatic for secretion retention, do the following:
- Oscillate
- Expectorate
- Ventilate
- If desired result not obtained, repeat from step 1.
Mucus vs. Phlegm
We often use the terms mucus and phlegm interchangeably, however, where the types of secretions originate from matter.
Mucus production tissue lines our upper airways and lower airways. Our upper airways include our nose and sinuses all the way down to our epiglottis, while our lower airways from our epiglottis down produce phlegm. When we have a cocktail mix of both sinus drainage, saliva and phlegm, we refer to that as sputum.
The characteristics of sputum samples, which more accurately are obtained via nasotracheal or endotracheal suction, can assist in identifying the type of microorganisms that have invaded our lungs. The goal is to stratify if the infection is viral or bacterial. It’s vital to obtain a good sample. The type of treatment, whether the patient will receive antibiotics or an antiviral, is dependent on the results. Clinicians note the consistency, color, smell (if applicable), and quantity of the sputum produced. By taking these factors into consideration and identifying the invader, clinicians are then able to strategize the best way to remove them from the lungs.
Oscillate
Our normal built-in oscillatory mechanism in our cardiopulmonary secretions is subtle, yet effective, for normal, compliant lungs. We refer to it as cilia. In a paper published in 2017 by Bustamante-Marin and Ostrowski, they describe cilia as “…specialized organelles that provide the force necessary to transport foreign materials in the respiratory tract toward the mouth where they can be swallowed or expectorated. To accomplish this crucial function, the cilia beat in coordinated metachronal waves at a beat frequency that has multiple physiological regulators.” We can imagine the cilia as an assembly line of workers transporting a heavy package from one end to the other. Instead of having one person take the heavy package from point A to point B, the assembly line works together to carry the load little by little. If that isn’t sufficient, the simple action of clearing our throat can create and mimic a beat frequency to assist in oscillating and bringing up those secretions.
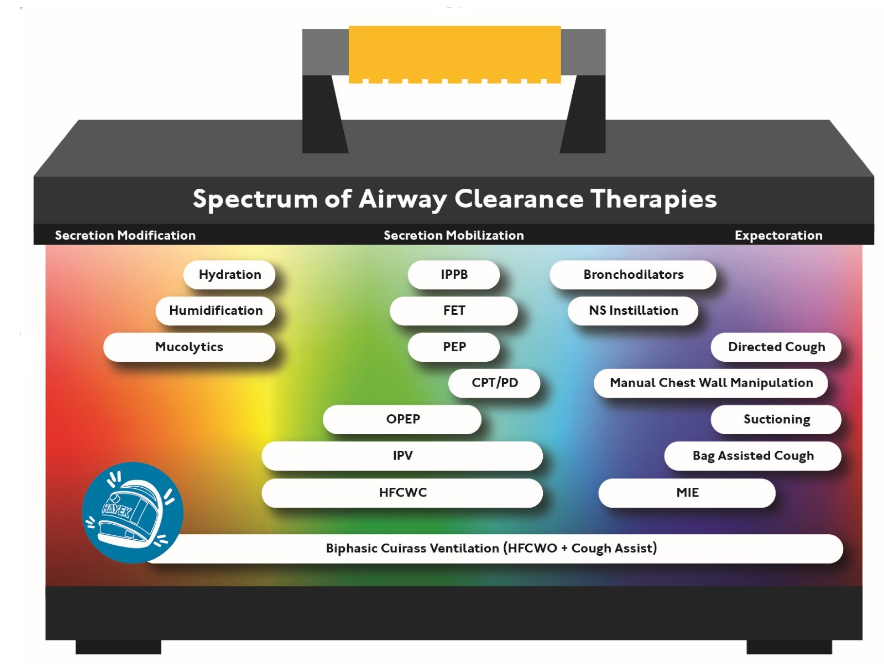
For many chronic disease processes, however, the cilia are compromised and unable to function to thin and to mobilize phlegm upward out of the lungs. In order to replicate the beat frequency produced by the metachronal waves, intrathoracic and extrathoracic oscillatory techniques have been developed. Examples of intrathoracic techniques include OPEP, IPPB, PEP, and IPV.
Extrathoracic techniques include high-frequency chest wall compression via air bladder vests or high frequency chest wall oscillators such as via the biphasic cuirass. One of the oldest, yet effective extrathoracic techniques include using a cupped hand for manual chest percussion. For those that choose manual chest percussion, postural drainage and positioning is key in helping secretions to naturally gravitate toward the large airways, making it easier to expectorate.
Expectorate
Once the phlegm is mobilized to the upper airways, it comes in contact with cough receptors located at the carina and lines the trachea, and the cough phase is initiated. The cough phase is made up of deep inspiration, glottic closure, pressure build-up in the lungs, glottic release, expiratory flow generation and it ends with secretion expulsion.
There are various chronic disease processes that impair this function as well, which include neuromuscular disorders and diaphragmatic paralysis. What techniques and mechanical processes have been invented to mimic our natural process? Controlled coughs and huff type cough have been effective techniques for those that do it appropriately. Mechanical support has also been accessible for many, which include intrathoracic assisted cough devices. An extrathoracic method that mimics our natural mechanism of a huff type cough would be via the biphasic cuirass.
Ventilate
Oftentimes, a large collection of phlegm, referred to as mucus plugs, will get plugged in the small airways and close off a functioning lung unit, causing atelectasis, decreasing FRC. Non-invasive ventilation, such as NIPPV, have been used for intrathoracic lung recruitment techniques to assist in restoring that FRC. As previously mentioned, a highly effective extrathoracic technique that mimics, yet again, our natural function is biphasic cuirass using continuous negative extrathoracic pressure. This can safely ventilate and restore any lost FRC from mucus plugs.
Conclusion
We have many options made available to us, the accompanying graphic discusses the spectrum techniques of airway clearance therapies available. We have the choice to use one, two, or three of them. However, taking into consideration our time, efficiency and the space allotted to us, why not use the one highly effective tool that covers the whole spectrum? Biphasic Cuirass Ventilation allows us the opportunity to use one interface to oscillate, expectorate, and ventilate.
Treating respiratory impairment with Biphasic Cuirass Ventilation (BCV) can include control, synchronized, and continuous negative extra-thoracic pressure (CNEP) to move intercostal muscles and diaphragm into a more normal physiological end expiratory position. This supportive negative pressure, which “holds open” opens the chest wall either cyclically or continuously depending on the mode used allows for the true source of most respiratory impairments to be corrected (volume loss). BCV enhances the natural negative trans-pulmonary pressure the body uses to create lung inflation.