The Glenn, and Fontan Procedure
Medical advancements have revolutionized the way we approach various health conditions, including congenital heart diseases. Among the surgical procedures aimed at addressing these conditions are the Glenn and Fontan procedures. These interventions have proven to be life-changing for patients and their families, providing hope and improved outcomes.
Understanding Congenital Heart Diseases
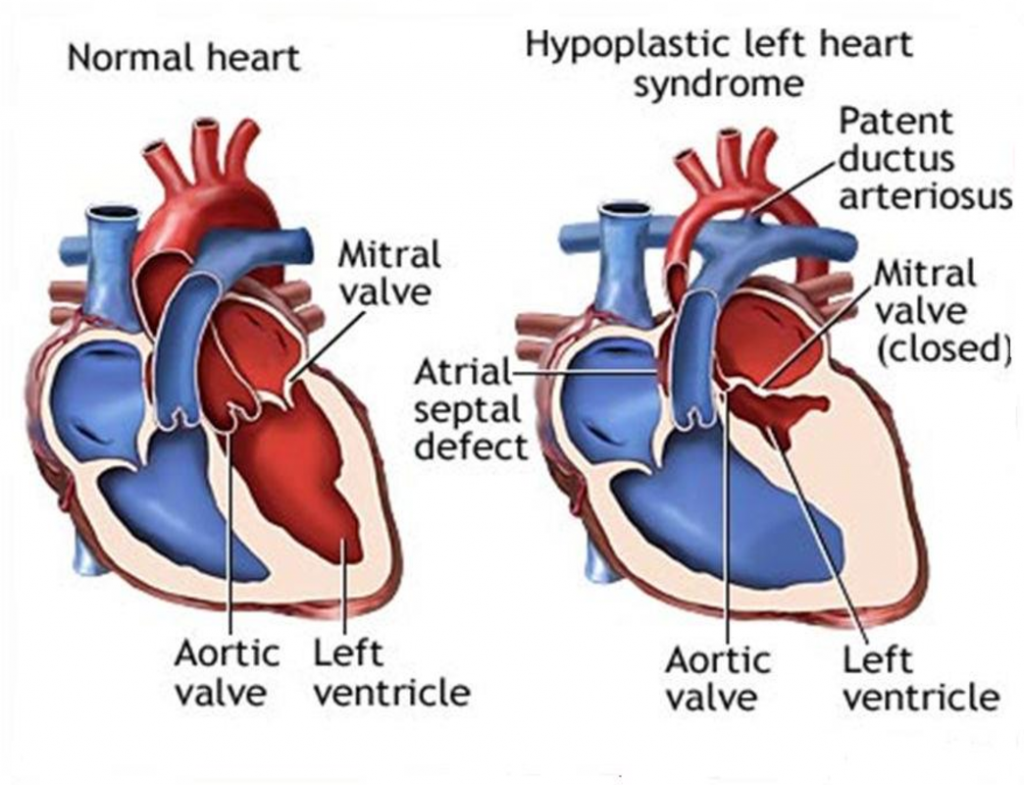
Congenital heart diseases encompass various conditions that affect the heart’s structure and function from birth. Many of these conditions involve abnormalities in the heart’s chambers, valves, or blood vessels, making it difficult for the heart to pump and circulate blood efficiently. In some cases, the heart may not have developed fully or be positioned correctly.
The Glenn and Fontan procedures are typically performed in patients born with single ventricle physiology, a condition that occurs when one of the ventricles, the pumping chambers of the heart, is either underdeveloped or nonfunctional. This results in an imbalance in blood flow, which can lead to complications and impaired oxygenation.
The Glenn Procedure: Improving Oxygenation
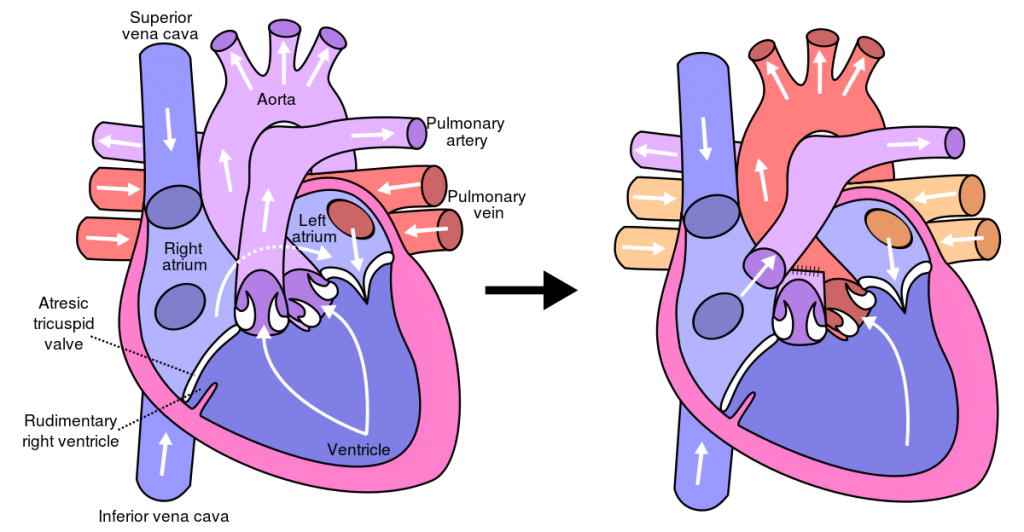
The Glenn procedure, also known as the superior cavopulmonary connection, is typically performed in infants around six to twelve months old. During this surgery, the superior vena cava, responsible for carrying deoxygenated blood from the upper body to the heart, is detached from the right atrium. The surgeon then redirects the blood flow directly to the lungs, bypassing the right ventricle completely.
By bypassing the right ventricle, the Glenn procedure helps improve oxygenation and reduces the workload on the heart. This surgical intervention allows for better circulation and alleviates symptoms like cyanosis, which is characterized by a bluish discoloration of the skin and mucous membranes due to low oxygen levels in the blood.
Benefits of the Glenn Procedure:
Following the Glenn procedure, patients experience improved oxygen saturation levels, reduced respiratory distress, and better overall cardiac function. Though this surgery is a significant milestone in the treatment of congenital heart diseases, it is often a step in a multi-staged surgical approach.
Results of the Glenn Procedure:
– Improved oxygen saturation levels
– Reduced respiratory distress
– Enhanced cardiac function
The Fontan Procedure: Optimizing Circulation
The Fontan procedure is the subsequent surgery performed after the Glenn procedure, usually between the ages of two and five. It involves rerouting the blood flow from the body directly to the pulmonary arteries, bypassing both ventricles. In this surgery, the inferior vena cava, responsible for carrying deoxygenated blood from the lower body to the heart, is detached from the right atrium and connected directly to the pulmonary arteries.
The purpose of the Fontan procedure is to complete the separation of systemic and pulmonary circulation, allowing deoxygenated blood to flow directly to the lungs for oxygenation. This surgical intervention helps to optimize blood flow, improve overall circulatory function, and reduce symptoms associated with congenital heart diseases.
Similar to the Glenn procedure, the Fontan procedure results in increased oxygen saturation levels, improved cardiac output, and decreased cyanosis. Patients who have undergone the Fontan procedure experience enhanced exercise tolerance and an improved quality of life.
Results of the Fontan Procedure:
– Increased oxygen saturation levels
– Improved cardiac output
– Decreased cyanosis
– Enhanced exercise tolerance and quality of life
Why use BCV For Post-Fontan Treatment?
In Fontan physiology, the lack of an active ventricular pump to deliver blood is a significant cause of decreased baseline Cardiac Output (CO) and Pulmonary Blood Flow (PBF). Limitations in CO in the Fontan population have primarily been attributed to increased pulmonary vascular resistance, ventricular dysfunction, and decreased afterload.
Due to the absence of the sub-pulmonary ventricle, the diaphragm is considered to be the most important inspiratory muscle for maintenance of venous return in the Fontan population. Respiration acts as a significant source of cardiac output in patients with Fontan physiology, and as such, findings of poor chest wall compliance, respiratory muscle weakness and restrictive lung physiology, which are commonly observed in the Fontan population, have significant impact on the cardiovascular flows of Fontan patients.
In treatment of post-fontan patients, it was found that:
- Implementation of negative pressure increased stroke volume, with no increase in heart rate.
- A brief period of cuirass NPV increased the pulmonary blood flow of patients with the Fontan circulation by 42%.
- The improvement in blood flow was not only sustained, but further continued if the period of NPV was extended.
Considerations and Risks of Glenn and Fontan Procedures:
Both the Glenn and Fontan procedures are intricate surgical interventions, with success depending on various factors, including the patient’s overall health, underlying heart conditions, and the surgeon’s expertise. As with any major surgical procedure, there are risks associated with these surgeries, including bleeding, infection, and complications related to anesthesia.
The Potential of a Fulfilling Life:
However, with advancements in surgical techniques, improved perioperative care, and ongoing research in the field of pediatric cardiology, the outcomes of these surgeries have significantly improved over the years. Many patients who undergo the Glenn and Fontan procedures go on to live fulfilling lives, participating in physical activities and enjoying a relatively normal life despite their underlying heart condition.
The Glenn and Fontan procedures have revolutionized the treatment of congenital heart diseases, specifically in patients with single ventricle physiology. These surgical interventions enhance blood flow, optimize oxygenation, reduce symptoms, and ultimately provide patients with an improved quality of life. As medical advancements continue, countless individuals and families can look forward to a brighter future.