A Brief History of Ventilation Therapies:
Negative Pressure Ventilation:
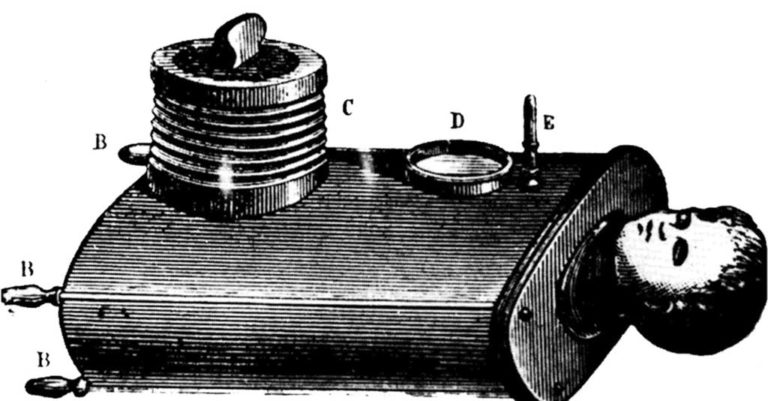
The first use of negative pressure ventilation appeared in 1838. Known as the “tank ventilator”, this allowed a patient to sit inside a box while only a person’s head remained outside open to ambient air. A pressure gauge was fitted to the outside of the box to read the level of negative pressure that was maintained by pumping air in and out through the use of a plunger to facilitate inspiration and expiration.
The Iron Lung: A Major Evolution
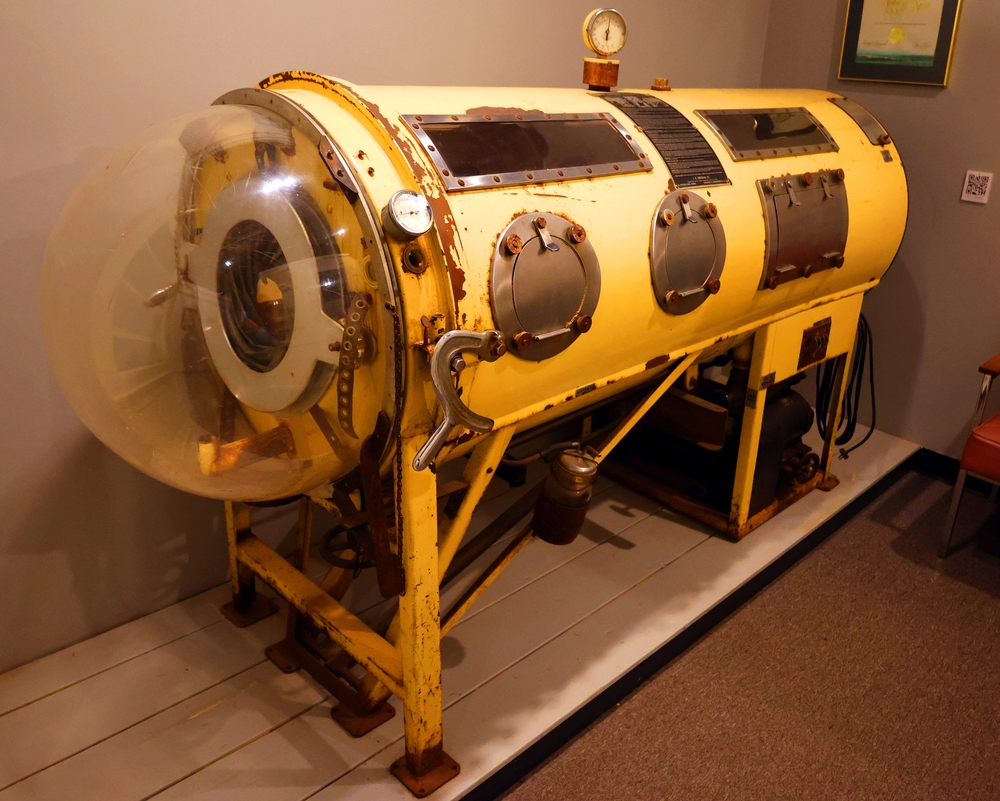
Fast forward to the invention of the iron lung, designed by Phillip Drinker and Louis Shaw, which was commonly used during the polio epidemic between 1930 and 1960. This cylindrical metal tube created negative pressure around the body of a supine patient, also leaving only the head open to ambient air thus allowing a person with weakened respiratory muscles from the disease to breathe easier. Although effective, the device had several drawbacks. Weighing in over 650 pounds, it was incredibly cumbersome. Access to the patient was through small portholes on the side of the device and made nursing and hygiene incredibly difficult.
Transition to Positive Pressure Ventilators
The iron lung began to be phased out with the advent of the modern day positive pressure ventilators such as the Bennett and Bird Mark series during the 1950’s. These pioneering models have evolved into the modern ventilators seen in the hospital today with a wide array of mode capabilities and portability for patients needing advanced care. However, ventilating the lung with positive pressure is not a natural method of breathing and can cause overdistention and trauma to the alveoli units within the lung.
Understanding Lung Damage from Positive Pressure
Damage caused to the lung by positive pressure was noted in postmortem patients as early as 1967 and was labeled “Respiratory Lung Syndrome”. The overdistention or stretching of alveoli within the lung caused by excessive volume/pressure followed by the subsequent reopening of these collapsed units with each breath can lead to the complication of barotrauma.
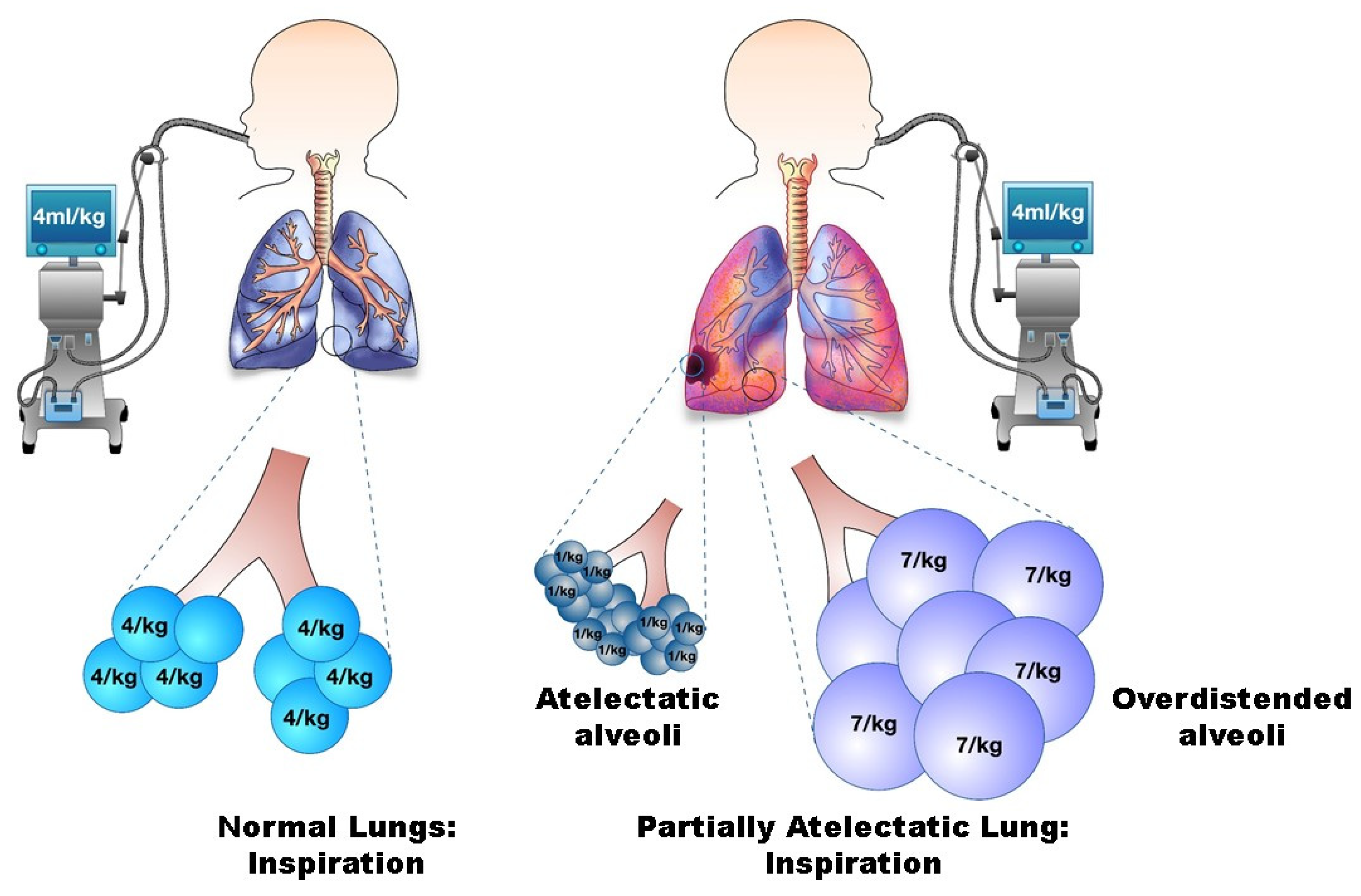
Barotrauma occurs when alveoli rupture and air enters into locations of the lung where it is not normally present. This cascading effect may lead to pneumothorax, pneumomediastinum, or subcutaneous emphysema. Lung protective measures and protocols used when initiating mechanical ventilation are the norm in hospitals today and are engineered to help prevent trauma to the lungs from high peak pressures. However, the mortality rate with patients who have prior comorbidities such as asthma, COPD, and interstitial lung disease are still significantly higher.
Costs Associated with Mechanical Ventilation
In 2009, the estimated cost of those requiring mechanical ventilation was $59,770 per patient. A 2019 study by Dexter and Scott noted that “more than 300,000 patients per year receive mechanical ventilation in the United States, and those who experience ventilator associated events developed a high morbidity and mortality risk,”
Complications from mechanical ventilation, whether infectious or noninfectious are proven to lengthen the hospital stay an average of seven to nine days.
Introduction to BCV
Negative pressure is the natural mechanism of breathing in humans and has evolved tremendously since the age of the iron lung. In 1995, Dr. Zamir Hayek introduced the Hayek biphasic cuirass ventilator (BCV) for use in pediatrics and adults. Through the use of a cuirass, which is worn over the thorax, the BCV creates negative pressure within the seal that allows for an easier work of breathing by allowing the rib cage to expand, lower the diaphragm, and allow atelectatic areas of the lung to reinflate. In addition to the negative pressure features of the device, the Hayek BCV also carries the capability to perform high frequency chest wall oscillation (HFCWO) with cough support to aid in secretion clearance.

Applications and Benefits of BCV
Use of the BCV has shown success avoiding the need for intubation by increasing Functional Residual Capacity (FRC), improving lung volumes and gas exchange, decreasing airway resistance, increasing cardiac output, and aiding with secretion clearance in a variety of patient populations such as:
· Neuromuscular disease (ALS, MS, MD)
· Pneumonia
· Spinal cord injury
· Congenital heart disease
· Asthma
· COPD
· Cystic Fibrosis
The BCV can be used as a noninvasive standalone unit. It may also work in conjunction with high flow therapy, mask ventilation, or together with mechanically ventilated patients in an effort to shorten ventilatory time.
A study published by Hassinger and colleagues in 2017 noted “a decline in the annual percentage of pediatric ICU admissions requiring intubation by 28% in the 3-year period following the introduction of negative pressure ventilation to their institution.”
While using the BCV, a person may eat, sleep, and talk unencumbered. A patient may use the device throughout the course of a hospital stay from ICU to discharge on a continuous or intermittent schedule and is FDA approved for use at home. Continued use of the BCV at home can decrease frequent recurring admissions and keep patients where they want to be -at home.
Cautions and Contraindications to BCV
Cautions and contraindications of BCV are far less than those associated with positive pressure ventilation using mask ventilation, endotracheal tubes, or tracheostomy tubes. These include:
· Weight greater than 180 kilograms.
· Burns or draining wounds under the shell or seal area.
· Indwelling lines or tubes directly underneath the foam around the shell.
· The lack of an airway whether natural or artificial.
· Cardiac arrest.
Improving outcomes
Avoiding the need for positive pressure ventilation and keeping patients as close to their baseline health as possible is a universal goal that all healthcare clinicians strive to achieve. Skyrocketing healthcare costs should drive the healthcare provider to use the earliest and most noninvasive interventions to avoid decompensation of patient populations which are already medically fragile.
Whether in use in an acute care setting or the home, the use of Biphasic Cuirass Ventilation with the Hayek has shown itself to be a novel yet cost effective and reliable approach to ventilation.