Despite significant advances in ventilator technology and standardized weaning protocols, ventilator weaning failure remains a common and complex issue in the ICU setting in 2025. Studies show that approximately 30-40% of technically ventilated patients experience difficult during the weaning process, particularly after prolonged ventilation periods.
The primary drivers of weaning failure can be categorized into three core areas: underlying pathophysiological conditions, clinical decision-making challenges, and systemic or iatrogenic complications.
Top 10 Causes of Ventilator Weaning Failure in 2025
BPD stems from underdeveloped lungs in premature infants. The condition is characterized by:
- Chronic Obstructive Pulmonary Disease (COPD)
Air trapping, dynamic hyperinflation, and ventilator asynchrony significantly impede respiratory recovery. - Congestive Heart Failure (CHF)
Pulmonary congestion increases the work of breathing and complicates weaning trials. - Neuromuscular Disorders
Conditions like ALS, Guillain-Barré syndrome, and Myasthenia Gravis impair muscular strength needed for spontaneous breathing. - Obesity Hypoventilation Syndrome (OHS)
Increased chest wall resistance, reduced respiratory drive, and rapid desaturation during spontaneous breathing trials. - Sepsis-Induced Respiratory Failure
Muscle catabolism, persistent systemic inflammation, and mitochondrial dysfunction hinder recovery of respiratory function. - Diaphragmatic Dysfunction
Often due to disuse atrophy or critical illness polyneuropathy, impairing the primary muscle of respiration. - Delirium or ICU-Acquired Weakness
These conditions reduce patient cooperation and voluntary respiratory effort. ICU acquired weakness is particularly common in prolonged ICU stays. - Acute Respiratory Distress Syndrome (ARDS)
Stiff, non-compliant lungs and positive end-expiratory pressure (PEEP) dependency make weaning risky and difficult. - Postoperative Respiratory Failure
Particularly after thoracic or upper abdominal surgeries due to pain, impaired diaphragmatic motion, or underlying complications. - Chronic Critical Illness / Syndrome of Prolonged Mechanical Ventilation (SPMV)
This multifactorial issue includes malnutrition, chronic inflammation, and endocrine imbalances, all of which delay ventilator liberation.
Disease-Specific Barriers to Weaning
A deeper look into three common patient profiles highlights how different factors influence weaning failure.
COPD Patients
Dynamic hyperinflation, ineffective gas exchange, and respiratory muscle fatigue contribute to weaning difficulty. Air trapping and the heightened effort of breathing post-extubation quickly exhaust weakened respiratory muscles.
Heart Failure Patients
Weaning trials can unmask underlying cardiac dysfunction. The transition from positive pressure ventilation to spontaneous breathing increases intrathoracic pressure fluctuations, elevating cardiac preload and afterload, leading to potential decompensation.
Sepsis Survivors
These patients often develop ICU-acquired weakness, including critical illness myopathy and neuropathy, severely affecting diaphragmatic function. Even with adequate oxygenation, neuromuscular fatigue may prevent successful spontaneous breathing.
Clinical warning signs of impending weaning failure include tachypnea, accessory muscle use, oxygen desaturation, CO₂ retention, and hemodynamic instability. Successful weaning requires early identification of risks, evidence-based weaning protocols, and prompt correction of reversible causes such as fluid imbalances, electrolyte disturbances, or oversedation.
How FRC Impacts Ventilator Weaning Failure
Functional Residual Capacity (FRC) is essential for oxygenation and lung volume stability during spontaneous breathing. Many patients fail to return to their baseline FRC due to:
- Atelectasis
- Muscle fatigue
- Loss of chest wall compliance
- Inadequate secretion clearance or weak cough
Without optimal FRC, patients develop poor gas exchange, rapid shallow breathing, and CO₂ retention, which often leads to reintubation or prolonged ventilator dependence.
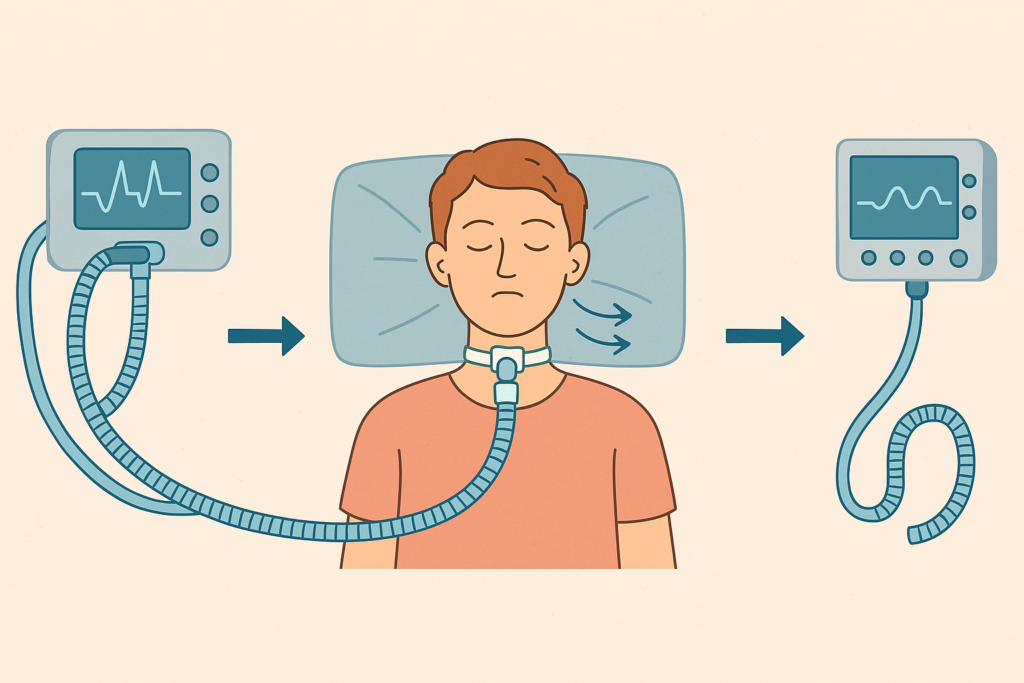
BCV: A New Tool to Reduce Ventilator Weaning Failure
Biphasic Cuirass Ventilation (BCV), a noninvasive negative-pressure ventilation method, is gaining renewed attention in 2025 for its unique ability to mimic natural breathing patterns. Unlike positive-pressure ventilation, BCV works externally and does not rely on airway-based triggers, making it especially useful in complex weaning scenarios.
Key BCV Benefits for Ventilator Weaning:
- Restores FRC noninvasively by re-expanding alveoli
- Reduces the work of breathing, especially in restrictive lung disease or obese patients
- Recruits posterior lung segments, ideal for supine ICU patients
- Improves secretion clearance using chest wall vibration or cough assist modes
- Reduces patient-ventilator dyssynchrony
- Prevents diaphragmatic disuse atrophy, encouraging natural breathing patterns
By restoring chest wall mechanics and improving ventilation-perfusion matching, BCV has the potential to shift the weaning paradigm—particularly in patients who have failed traditional methods.
Final Thoughts
Mechanical ventilation weaning failure remains a pressing issue, even in 2025. But with better awareness of disease-specific challenges, early risk identification, and emerging noninvasive tools like BCV, clinicians can offer patients a more personalized path to ventilator liberation.